The landscape of nursing licensure examination has fundamentally changed. Since April 2023, the Next Generation NCLEX (NGN) has made clinical judgment the centerpiece of every exam, transforming how nursing candidates must prepare for their licensure journey. This isn’t just an update—it’s a complete paradigm shift that rewards critical thinking over memorization.
For Filipino nurses preparing to work in the United States, understanding clinical judgment has become more critical than ever. With International Educated Nurse (IEN) pass rates hovering between 47-54%, mastering the clinical judgment framework can mean the difference between achieving your nursing career goals and facing repeated examination attempts.
At Ray A. Gapuz Review System (RAGRS), we’ve maintained a 100% pass rate since 2001 by continuously evolving our teaching methods to match NCLEX requirements. Our syndromic approach to nursing education directly develops the clinical reasoning skills the NGN now measures. In this comprehensive guide, you’ll discover exactly what clinical judgment means on the NCLEX, master the 6-step framework that underlies every NGN question, understand each new question type, and learn proven strategies that have helped thousands of Filipino nurses achieve their American nursing dreams.
Let’s dive into everything you need to know about clinical judgment on the 2026 NCLEX examination.
What is Clinical Judgment on the NCLEX?
The Shift from Knowledge to Judgment
The traditional NCLEX rewarded nurses who could memorize vast amounts of information: drug dosages, normal lab values, disease symptoms. While this knowledge remains essential, the NGN format recognizes a fundamental truth about nursing practice—knowing facts isn’t the same as making sound clinical decisions.
Consider two nurses who both know that a patient’s potassium level of 6.2 mEq/L is dangerously elevated. One nurse recognizes this as an isolated fact. The other nurse immediately connects this finding to the patient’s renal function, current medications, ECG rhythm, and overall clinical picture—then takes appropriate action. The NGN was designed to identify and reward the second type of nurse.
This shift reflects real-world patient care demands. Hospital administrators and nursing boards worldwide agree: nurses who can synthesize information, prioritize effectively, and make sound decisions under pressure provide safer patient care. The NCLEX now measures these abilities explicitly.
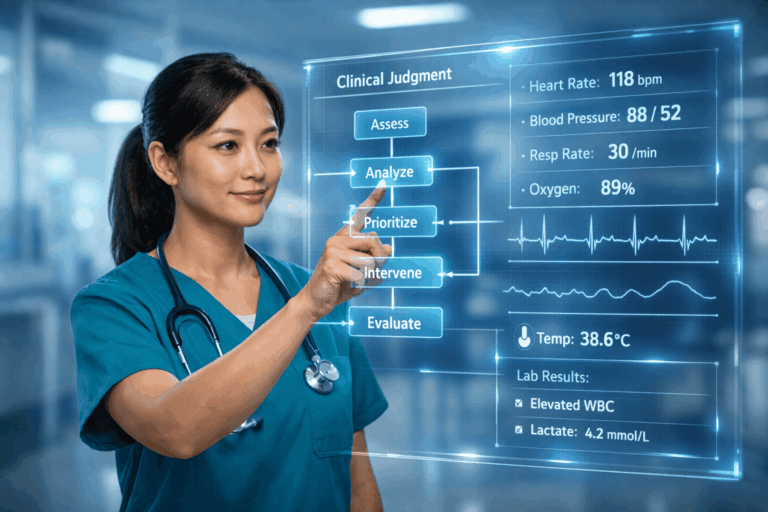
The NCSBN Clinical Judgment Measurement Model (NCJMM)
The National Council of State Boards of Nursing (NCSBN) developed the Clinical Judgment Measurement Model as the theoretical foundation for NGN questions. This evidence-based framework identifies six cognitive skills that competent nurses use when making clinical decisions:
- Recognize Cues — Identifying relevant patient information
- Analyze Cues — Understanding what the information means
- Prioritize Hypotheses — Ranking potential patient problems
- Generate Solutions — Identifying possible interventions
- Take Action — Selecting the best intervention
- Evaluate Outcomes — Assessing whether the intervention worked
Every NGN question, whether a single item or part of a case study, measures one or more of these skills. Understanding this framework transforms how you approach practice questions and helps you think like the expert nurses who pass on their first attempt.
The 6-Step Clinical Judgment Framework
Step 1 — Recognize Cues
Clinical judgment begins with observation. Before you can analyze a patient situation, you must first identify the relevant pieces of information—the cues that signal what’s happening with your patient.
What are cues in nursing scenarios?
Cues include:
- Objective data: Vital signs (BP 180/110, HR 48, SpO2 88%), lab values (K+ 6.2, Hgb 7.1), physical assessment findings
- Subjective data: Patient statements (“I feel like I can’t catch my breath”), reported symptoms, pain descriptions
- Environmental factors: Isolation status, equipment connections, positioning
- Historical information: Medical history, recent procedures, current medications
Common mistakes to avoid:
- Treating all information as equally important
- Missing subtle but critical changes in patient status
- Overlooking patient statements in favor of numerical data
- Failing to compare current findings to baseline values
Practice tip: When reading NCLEX case studies, mentally highlight the 3-5 most clinically significant pieces of information before looking at the question.
Step 2 — Analyze Cues
Recognition without understanding leads nowhere. Analysis means connecting the dots between individual data points to form a coherent clinical picture.
The key question: “What does this mean for the patient?”
When you see a potassium level of 6.2 mEq/L, analysis means asking:
- Why is this happening? (Renal failure? Medication side effect? Tissue breakdown?)
- What are the immediate risks? (Cardiac arrhythmias, cardiac arrest)
- How does this connect to other findings? (Check the ECG, assess renal function, review medications)
Identifying relevant vs. irrelevant information:
NGN questions deliberately include distracting information. The skilled test-taker learns to distinguish between:
- Relevant: Information that affects immediate care decisions
- Background: Information that provides context but doesn’t change your approach
- Irrelevant: Information included to test your ability to focus
RAGRS syndromic connection: Our teaching approach emphasizes pattern recognition—identifying clusters of findings that point to specific conditions or complications. This directly builds the analytical skills the NGN measures.
Step 3 — Prioritize Hypotheses
Patients rarely present with single, isolated problems. Competent nurses develop multiple working hypotheses about what might be happening and rank them by urgency and likelihood.
Forming nursing diagnoses:
Based on your cue analysis, identify the potential patient problems. For a patient with elevated potassium, possible hypotheses include:
- Acute kidney injury causing electrolyte imbalance
- Medication-induced hyperkalemia
- Diabetic ketoacidosis with potassium shift
- Laboratory error requiring repeat testing
Ranking by urgency using established frameworks:
ABCs (Airway, Breathing, Circulation): Life-threatening issues always come first
- Airway obstruction takes priority over breathing problems
- Breathing problems take priority over circulation issues
- Circulation problems take priority over other concerns
Maslow’s Hierarchy: For non-emergency prioritization
- Physiological needs first (oxygen, circulation, elimination, nutrition)
- Safety needs second (preventing falls, avoiding medication errors)
- Psychosocial needs after physiological and safety are addressed
Step 4 — Generate Solutions
With your prioritized hypotheses established, identify the range of possible interventions. This step requires broad nursing knowledge and understanding of evidence-based practice.
Key considerations when generating solutions:
- What interventions address the highest-priority problem?
- Which actions are within the nurse’s scope of practice?
- What does evidence-based practice recommend?
- Are there contraindications to consider?
For our hyperkalemic patient, potential solutions include:
- Administer calcium gluconate for cardiac protection
- Give insulin with dextrose to shift potassium intracellularly
- Administer sodium polystyrene sulfonate (Kayexalate) to eliminate potassium
- Prepare for emergency dialysis
- Discontinue potassium-sparing medications
- Obtain STAT ECG and place on continuous cardiac monitoring
The RAGRS syndromic approach advantage: Our teaching method builds extensive solution libraries organized by clinical presentation, helping students quickly generate appropriate intervention options.
Step 5 — Take Action
This is where clinical judgment becomes clinical practice. Among all possible solutions, you must select the BEST one for this specific patient in this specific situation.
Understanding “most appropriate” language:
NCLEX questions often ask for the “most appropriate” or “priority” action. This doesn’t mean other options are wrong—it means one option is BEST given the circumstances. Consider:
- Timing: What needs to happen first?
- Patient-specific factors: What makes this patient unique?
- Resources: What’s available and appropriate?
- Scope of practice: What can you do independently?
Delegation and prioritization in action:
When multiple actions are needed:
- Prioritize by patient safety and ABC principles
- Delegate appropriately to available staff
- Perform assessments before interventions (usually)
- Document after stabilizing the patient
Step 6 — Evaluate Outcomes
Clinical judgment doesn’t end with intervention—it requires ongoing assessment of whether your actions achieved the desired effect.
Assessing intervention effectiveness:
- Did the patient’s condition improve?
- Are vital signs trending toward normal?
- Has the immediate threat been addressed?
- Are there new problems developing?
When to reassess and modify:
- If the expected improvement doesn’t occur within the anticipated timeframe
- If new symptoms or complications develop
- If the patient’s condition changes significantly
Documentation considerations:
- Record baseline assessment, intervention, and patient response
- Note timing of reassessment
- Document any modifications to the care plan
NGN Question Types You’ll See on NCLEX 2026
Case Studies (Unfolding Scenarios)
The most significant NGN change involves case studies—multi-part scenarios that follow a single patient through an evolving clinical situation.
Structure:
- 3 scored case studies per exam (plus unscored field test items)
- 6 questions per case study (18 total case study questions)
- Questions follow the patient through time, with new information revealed
- Earlier answers may influence later questions within the same case
How to approach them systematically:
- Read the initial scenario carefully—twice if needed
- Note key patient details: age, diagnosis, relevant history
- Answer each question based on the information available at that point
- Expect the situation to evolve (improve or deteriorate)
- Apply the 6-step framework to each question
New Item Typesqq
| Question Type | Description | Strategy |
|---|---|---|
| Extended Multiple Response | Enhanced “select all that apply” with more options | Evaluate EACH option as true/false independently |
| Extended Drag and Drop | Order or categorize multiple items | Identify the priority sequence or categories first |
| Cloze (Drop-down) | Complete sentences by selecting from dropdown menus | Context clues are essential—read the full sentence |
| Matrix/Grid | Multi-dimensional tables with multiple selection points | Check BOTH rows AND columns for accuracy |
| Enhanced Hot Spot | Select specific areas on images or diagrams | Anatomy review is essential for success |
| Highlight | Mark relevant portions of text | Focus on clinically significant information |
How to Practice Clinical Judgment Skills
Study Strategies That Work
Active case analysis vs. passive reading: Don’t just read case studies—actively engage with them. Before looking at questions, write down:
- The 3-5 most important findings
- Your working hypothesis
- Your priority intervention
Then compare your thinking to the question requirements.
The “Think Aloud” method: Verbalize your clinical reasoning as you work through practice questions. Explain why you’re eliminating options and selecting answers. This builds metacognitive awareness of your decision-making process.
RAGRS syndromic approach application: Our course teaches pattern recognition—identifying clusters of findings that point to specific conditions. Practice applying this approach to every practice scenario.
Recommended Practice Resources
- Official NCSBN practice exams: The most accurate representation of actual NGN questions
- RAGRS review materials: Specifically designed for Filipino nurse success
- Quality question banks: Choose resources with detailed rationales explaining the clinical reasoning
Common Mistakes to Avoid
- Overthinking simple scenarios: Not every question requires complex analysis
- Ignoring patient safety priorities: When in doubt, choose the safest option
- Rushing through case studies: Take time to understand the full clinical picture
- Memorizing answer patterns: Focus on understanding reasoning, not recognizing question types
April 2026 NCLEX Updates: What’s Changing?
New Test Plan Highlights
The NCSBN releases updated test plans every three years. The April 2026 updates include:
- Updated activity statements: Refined descriptions of nursing activities being tested
- Terminology updates: “Substance Misuse” replaces older terminology throughout
- Enhanced clinical judgment emphasis: Even more focus on decision-making skills
- Integrated process categories: Content organized around nursing processes rather than disease conditions
What’s NOT Changing
- Computer Adaptive Testing (CAT): The exam still adapts to your performance level
- 5-hour time limit: Total examination time remains constant
- Question count: 70-135 questions for RN (still variable based on performance)
- Passing standard: The NCSBN maintains consistent competency requirements
RAGRS Clinical Judgment Success Stories
For over three decades, Ray A. Gapuz Review System has prepared Filipino nurses for NCLEX success. Our 100% pass rate since 2001 reflects our commitment to developing the clinical reasoning skills that modern nursing demands.
Why our syndromic approach works for clinical judgment:
Our methodology teaches nurses to recognize clinical patterns—clusters of findings that point to specific conditions or complications. This pattern-recognition approach directly develops the cue recognition and analysis skills that NGN questions measure.
Students who complete our program report feeling confident when facing case study questions because they’ve practiced the systematic thinking process throughout their preparation. They approach unfamiliar scenarios with a framework, not fear.
Frequently Asked Questions
1. What percentage of NCLEX questions involve clinical judgment?
Clinical judgment is assessed throughout the entire exam, not just in specific questions. Approximately 22-33% of scored items come from case studies (18 questions from 3 case studies), but clinical reasoning is embedded in standard questions as well.
2. How long should I study for NGN questions specifically?
Most students need 8-12 weeks of focused preparation, with daily practice on case study scenarios. However, clinical judgment isn’t a separate skill—it develops through consistent application of systematic thinking to all practice questions.
3. Is clinical judgment harder for international nurses?
Filipino nurses may need additional practice with U.S. healthcare context and terminology, but the underlying clinical reasoning skills are universal. Strong nursing education in the Philippines provides an excellent foundation for clinical judgment.
4. What if I struggle with clinical judgment questions?
The CAT adapts to your performance level. Rather than worrying about individual questions, focus on consistently applying the 6-step framework. Each question is an opportunity to demonstrate your reasoning ability.
5. Can I use ChatGPT or AI tools to practice clinical judgment?
AI tools can supplement your study by explaining concepts, but they cannot replace structured practice with validated NCLEX-style questions. The nuanced clinical reasoning required exceeds what current AI reliably provides—stick with reputable practice resources.
6. How do I know if I’m ready for clinical judgment questions?
Consistent performance of 65% or higher on practice case studies indicates readiness. RAGRS offers diagnostic assessments that evaluate your clinical reasoning skills and identify areas needing additional focus.
7. What’s the current IEN pass rate for the NGN format?
International Educated Nurse first-time pass rates range from 47-54%, compared to approximately 79% for U.S.-educated candidates. Targeted preparation focusing on clinical judgment can significantly improve these outcomes.
8. Does RAGRS specifically teach clinical judgment skills?
Absolutely. The RAGRS syndromic approach directly develops clinical decision-making abilities. Our curriculum integrates clinical judgment throughout every topic, not as a separate module but as a fundamental thinking framework.
Your Clinical Judgment Journey Starts Here
Clinical judgment isn’t just an exam requirement—it’s the foundation of safe, effective nursing practice. The skills you develop preparing for the NGN will serve you throughout your nursing career, helping you make sound decisions that protect your patients and advance your profession.
The 6-step framework, once internalized, becomes automatic. You’ll find yourself recognizing cues, analyzing patterns, and prioritizing interventions without conscious effort—exactly as expert nurses do.
At Ray A. Gapuz Review System, we’ve spent over 30 years perfecting our approach to NCLEX preparation. Our syndromic teaching method was built on clinical reasoning principles long before the NGN made them explicit examination requirements. We don’t just prepare you to pass—we prepare you to practice.
Ready to master clinical judgment? Contact RAGRS today to learn how our proven approach can accelerate your path to NCLEX success and your American nursing career.